A series of large-scale genomic studies has reported that clonally expanded hematopoietic cells bearing somatic mutations are increasingly prevalent with age, even in the absence of cytopenias, myelodysplasia, or leukemia. Individuals with acquired somatic mutations at a variant allele frequency (VAF) of at least 2% in genes recurrently mutated in hematologic malignancies not meeting criteria for any known hematologic disorders have been labeled as manifesting "age-related clonal hematopoiesis (ARCH)". Dominant negative or loss-of-function (LOF) mutations in genes encoding for epigenetic modifier enzymes such as DNMT3A, TET2, and ASXL1 are most common in ARCH, and individuals with ARCH are at a greater risk for cardiovascular diseases as well as hematologic malignancies. However, the relationships between these mutations, clonal expansion, and clinical outcomes are not fully elucidated due to difficulties in studying individuals with ARCH longitudinally over time in the absence of an overt clinical abnormality, and extrapolating from murine models that may not closely recapitulate human hematopoietic physiology. Since non-human primates (NHP) have a high similarity in HSPC and marrow properties to humans, and we have identified typical spontaneous ARCH mutations in aged macaques not yet identified in aged mice, we sought to generate a rhesus macaque model of human ARCH utilizing CRISPR/Cas9 technology to investigate clonal behavior and intervention strategies.
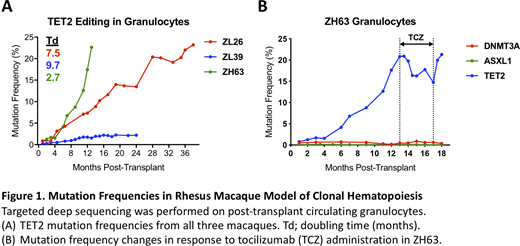
We delivered a gRNA pool targeting the three most frequently mutated genes in human ARCH with Cas9 in the form of ribonucleoprotein (RNP) into HSPCs obtained from three young adult macaques, targeting a low efficiency, and the edited HSPCs were reinfused into autologous animals following total body irradiation. All macaques engrafted promptly after transplantation and maintained normal blood counts. Up to three years of long-term follow-up revealed reproducible and significant expansion of multiple HSPC clones with heterozygous TET2 LOF mutations, compared to the limited expansion of clones carrying DNMT3A and ASXL1 mutations, reaching a VAF almost 25% with doubling time of 7.5 months in circulating granulocytes of the first macaque (ZL26, Fig 1A). Although there were differences in population doubling rates between individuals, the three macaques shared the general pattern of a gradual but dramatic expansion of TET2-mutated clones, with most of the expanding indels resulting in frameshifts predicted to result in LOF. These data suggest a single mutation in TET2 is sufficient for clonal expansion, and that other intrinsic and/or extrinsic factors can regulate the pace of TET2 clonal expansion. Bone marrow of these macaques exhibited hypercellularity and myeloid-predominant skewing without dysplastic changes compared with macaques of similar age previously transplanted with HSPCs edited at non-ARCH loci. Furthermore, RNA-seq indicated that TET2-disrupted myeloid colony-forming units (CFUs) and mature cells exhibited a distinct hyperinflammatory gene expression profile. Indeed, CD14+CD163+ macrophages purified from all three ARCH macaques exhibited hyperinflammatory function, with upregulated NLRP3 inflammasome activity and increased IL-6 signaling. We hypothesized that interrupting the vicious cycle of clonal expansion driven by and driving inflammation could halt the expansion of TET2-mutated clones. To address this, we treated the animal with the fastest TET2-mutant clonal expansion (ZH63) with tocilizumab, an antibody blocking IL-6 signaling, starting 13 months after transplantation and continuing for 4 months. The TET2 mutated allele frequency in granulocytes declined by 30% by the end of the treatment and began to increase again after withdrawal (Fig 1B), suggesting that interruption of the IL-6 axis removes the selective advantage of mutant HSPCs and this repressive effect is specific to the TET2-mutant genotype.
In summary, our CRISPR/Cas9-engineered rhesus macaque ARCH model recapitulates human ARCH and uncovers the impact of TET2 LOF on hematopoiesis and inflammation, as well as demonstrates the suppressive effect of IL-6 axis blockade in TET2-mutant clonal expansions. This robust NHP model will be further utilized for examining the pathophysiology of ARCH and testing of potential therapeutic interventions.
Dunbar:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal